“When I first heard the terms ‘portable’ and ‘MRI’ together, I did a double take,” said W. Taylor Kimberly, MD, PhD, chief of the Division of Neurocritical Care and a stroke and critical care neurologist in the Department of Neurology at Mass General Brigham (MGB). “I thought to myself, ‘How is this even possible?’”
That was nearly eight years ago. Since then, researchers at the Athinoula A. Martinos Center for Biomedical Imaging at Massachusetts General Hospital, led by Matthew S. Rosen, PhD, and J. Eugenio Iglesias, PhD, have been refining their low-field MRI technology and artificial intelligence (AI) tools to improve image quality and working with clinician champions such as Kimberly to bring it to the bedside.
Kimberly believes the technology has the potential to redefine how neurological conditions are diagnosed and monitored both within MGB’s Neuroscience Institute and in under-resourced communities.
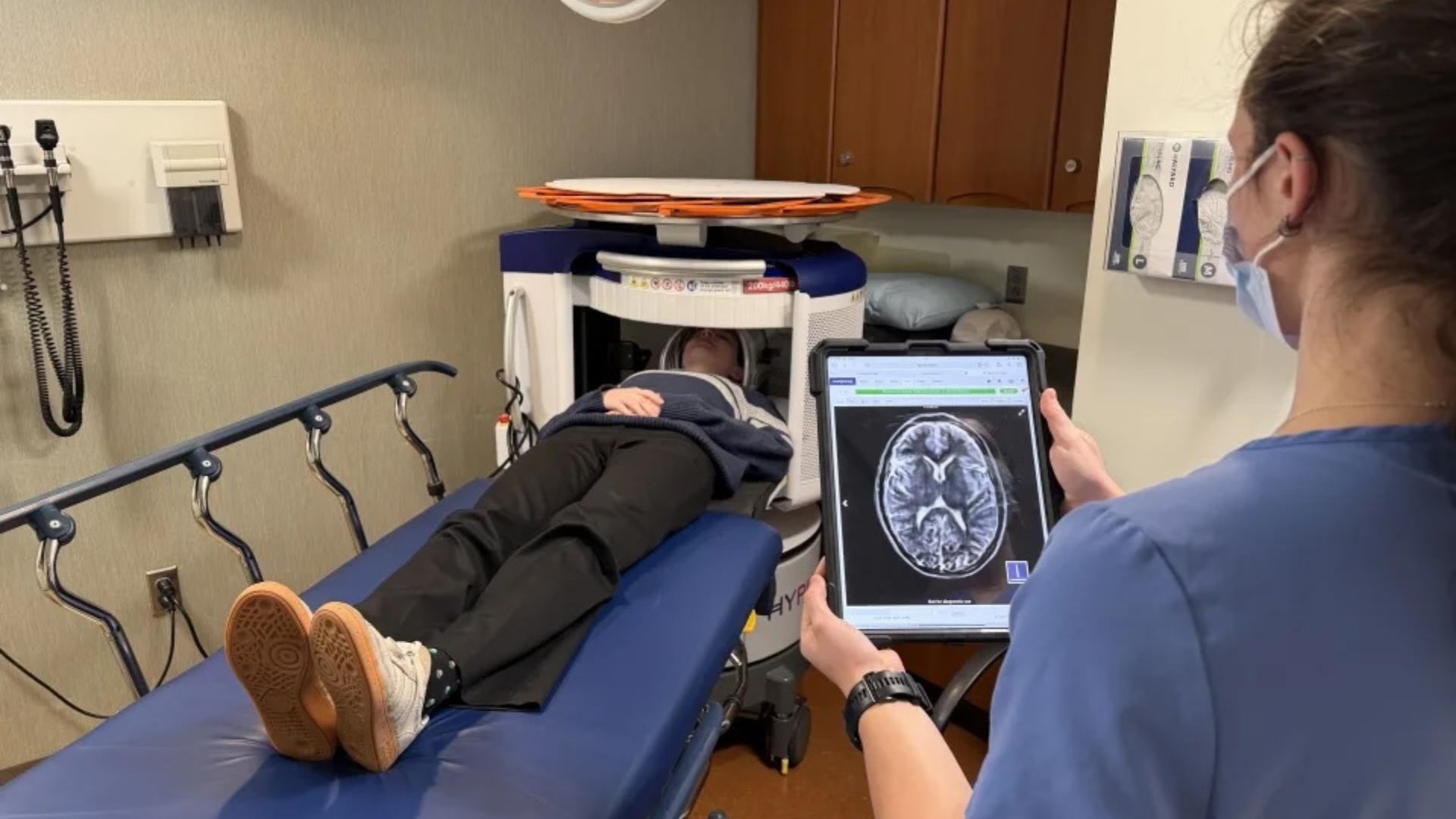
“Conventional MRI produces amazing, exquisitely detailed images that we use to diagnose and monitor neurological and neurosurgical conditions. But the scanner needs to be cooled with liquid helium and liquid nitrogen, it weighs thousands of pounds and it has to be isolated from radiofrequency noise that is always in the environment. And, because of the high magnetic field strength, there are safety protocols to which we must strictly adhere. That leads to a limitation in access to conventional MRI,” he said. “In comparison, portable MRI turns that paradigm on its head. The technology requires two large planar static magnets, positioned so that a head can fit between them, installed on motorized wheels with a computer. By plugging the scanner into a regular electrical outlet, you can derive images for diagnosis and monitoring. The images are not as high quality as those produced by conventional MRI, but with machine learning and AI, year after year, they are getting closer and closer in quality.”
Kimberly sees several use cases for portable MRI technology that open up new avenues for diagnosis and monitoring when conventional MRI is impractical or unavailable.
At the bedside, portable MRI can be used to obtain images for patients who are too sick to travel to the conventional MRI suite. “I see this with my neurocritical care patients all the time,” Kimberly said. “We need the images to help determine the plan of care, but we just can’t safely transport the patient to another area of the hospital.”
In the Emergency Department, the use of portable MRI can speed diagnosis of the patient’s ailment, particularly when it comes to stroke. “The majority of stroke cases that present in the Emergency Department, particularly in our community hospitals, are small strokes or TIAs (transient ischemic attack). Often patients wait hours for a diagnostic MRI in these cases. We think portable MRI has the potential to reduce length of stay in the Emergency Department by giving clinicians the information they need, rapidly, to determine if the patient needs to be admitted to the hospital, transported to another facility or can be safely discharged home,” Kimberly said.
In the community, portable MRI scanners can be quickly mobilized and delivered to areas where conventional MRI is unavailable. “Here in the Northeast, we are lucky to have conventional MRI technology fairly accessible,” said Kimberly. “But in other parts of this country and around the world, it’s not as common.”
In the clinic, portable MRI can be installed in a standard exam room, allowing clinicians to order imaging during a patient visit. This makes appointments far more comfortable and efficient for patients, who can now meet with their provider and complete imaging in a single visit, eliminating the stress and inconvenience of multiple trips to different locations. “For memory care patients and their families, this can be extremely helpful,” said Teresa Gomez-Isla, MD, PhD, chief of the Division of Memory Disorders in the Department of Neurology at MGB. “I can walk my patient to the MRI next door, stay with them during the scan and go over the results together immediately afterward. While it does not yet replace the full capabilities of a standard MRI, it transforms the patient’s experience, making visits smoother, less stressful and truly centered on the individual. For patients and families, this means care that is seamless, compassionate and responsive, where science and humanity come together in every step of the journey.”
Two key areas of focus for the MGB Neuroscience Institute are to keep the patient at the center and to foster new ideas and technology within the neurosciences. Advancing portable MRI technology and its availability does both.
“This is truly patient-centered technology. It’s convenient for the patient and it provides information at the point of care for the clinician. And it does so in a cost-effective and simple-to-operate manner,” Kimberly said. “In the future, as the technology is more widely adopted, we hope to use it as part of a one-stop brain health assessment, which includes this bedside imaging, a screening cognitive assessment and blood biomarkers for Alzheimer disease. It’s a scalable, streamlined way to assess brain health and inform subsequent treatment plans.”
This article originally appeared in the MGB Vitals newsletter. Reprinted courtesy of author Stephanie Brooks of MGB Internal Communications.